Womens Health
Medical Certificates
 MEDICAL CERTIFICATES
MEDICAL CERTIFICATES
(WORK, EXAMS, SCHOOL)
If you are unable to attend work, exams or school you may be required to provide a medical certificate. This can be obtained by visiting the doctor and by proving that you are sick or unfit for work, school or exams.
Mental Health Plans
Mental Health Plans

A Mental Health Care Plan is a plan made by your doctor for treating a mental health problem over time.
Your Doctor will work with you to assess your mental health, work out what help you need, set goals and choose the treatment that would be best for you. Your doctor will also discuss options for treatment and advise you about any other services that might help you. (The plan might also include what to do in a crisis or to prevent relapse.)
Once you and your doctor have agreed on your goals and what you need to do to achieve them, your doctor will write out a mental health care plan. Preparing the plan may take a number of visits.
Allergies
Allergies
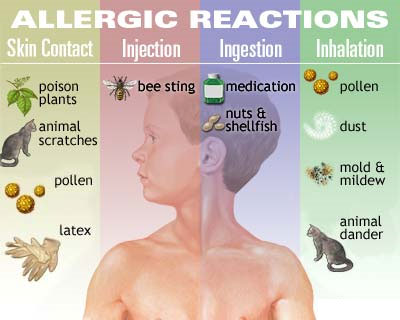
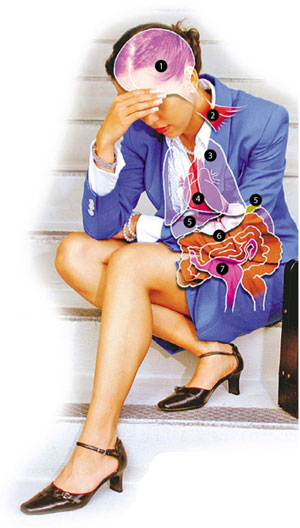
An allergy is an abnormal reaction by a person's immune system against a normally harmless substance. A person without allergies would have no reaction to this substance, but when a person who is allergic encounters the trigger, the body reacts by releasing chemicals which cause allergy symptoms. However, just because there is a cause and effect between exposure to a substance and the development of symptoms does not always mean that a person is allergic to that substance.
Allergies can be:
- Nasal Allergies
- Hay Fever
- Skin Allergies
- Food Allergies
- Drug and Medicine Allergies
- Insect Allergies
If you think you may have had an allergic reaction.

This little boy is suffering severe facial swelling and urticaria.
These are not life-threatening in themselves but may lead to more severe symptoms, such as anaphylaxis.

EpiPen® Auto-Injector is the #1 doctor prescribed epinephrine Auto-Injector for those with a history of anaphylaxis. EpiPen® helps stop allergic reactions fast - giving you time to get the emergency medical help you need.
Infections
Infections
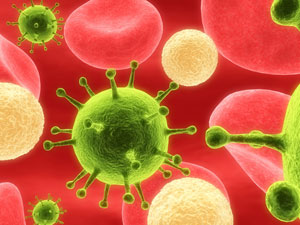
Many human illnesses are caused by infection with either pathogenic (disease-causing) bacteria or viruses. To cause disease, these micro-organisms must gain access to the body. Bacteria reproduce by splitting in two, while viruses replicate themselves inside host cells. Many bacterial infections can be treated successfully with antibiotics, but these are useless against viral infections.
Types of Infections
- Skin
- Eye Infections
- Viral Infections
- Ear Infections
- Wound Infection
- Urinary Tract Infections
- Bacterial Infections
- Kidney Infections
- Chest Infections
- Stomach Infections
- Fungal Infections
- Cold and Flu
- Lung and Respiratory
- Parasitic Infections
Cervical Screening (Pap Smear )
Cervical Screening (Pap Smear)
Our Doctors or Registered Nurses can perform a Pap Smear to look for cervical and/or vaginal cells that are cancerous or could be potentially pre-cancerous. The Pap test can also be used to detect vaginal or uterine infections.
Please talk to your doctor about having a pap smear test.
The Nation Cervical Screening Program promotes routine screening with Pap smears every two years for women between the ages of 18 (or two years after first sexual intercourse, whichever is later) and 69 years..

The Program seeks to integrate all elements of the cervical screening process. In particular, it aims to:
- demonstrate an increase in the percentage of eligible women who have ever been screened;
- establish more reliable and accessible services for taking, interpreting and reporting Pap tests;
- improve management of screen detected abnormalities; and
- monitor and evaluate these preventive efforts.
The Program includes: implementation and monitoring of adherence to a nationally agreed screening policy; establishment of Pap test registers in Qld and development and enhancement of other quality management strategies across the screening pathway.
The screening pathway involves the following steps:
- encouraging all eligible women to enter and remain in the screening program;
- ensuring optimal quality of Pap smears by adequate training of Pap smear takers;
- ensuring optimal quality of Pap smear reading through a quality assurance program for laboratories;
- ensuring appropriate follow up of abnormal Pap smears through management guidelines;
- providing an efficient system for notifying results to women by Pap smear providers;
- providing recall and reminder systems to ensure adequate follow up of women with screen-detected abnormalities; and
- maintaining women’s participation in the program by encouraging providers to set-up reminder systems, and developing cervical cytology registers and national cancer data.
Sexually Transmitted Infection Screening
Sexually Transmitted Infection Screening
Sexually transmitted diseases (STDs) are infections that you can get from having sex with someone who has the infection. The causes of STDs are bacteria, parasites and viruses. Some Types of these diseases are Chlamydia, Gonorrhea (The Clap), Pelvic Imflammatory Disease, HPV, Syphilis, Herpes Simplex HSV, Trichomoniasis,
Rates of sexually transmitted infections are increasing worldwide and notifications are also increasing in Australia. As many sexually transmitted infections are asymptomatic, timely and appropriate testing is needed to avoid the long-term sequel of infection, to halt transmission. Testing for sexually transmitted infections has evolved over time. Although nucleic acid amplification tests have an increasing role and may enable non-invasive testing, microscopy and culture are still useful investigations for some infections.
Bacterial Vaginosis (BV)
Bacterial Vaginosis (BV)

The vagina normally has a balance of mostly good bacteria and fewer harmful bacteria. Bacterial vaginosis develops when the balance changes. With Bacterial Vaginosis there is an increase in harmful bacteria and a decrease in good bacteria. Bacterial Vaginosis is the most common vaginal infection in women of childbearing age. Not much is known about how women get Bacterial Vaginosis, There are certain things that can upset the normal balance of bacteria in the vagina, raising your risk of Bacterial Vaginosos and these can include having a new sex partner or multiple sex partners, douching, using an intrauterine device for birth control and not using a condom.
Bacterial Vaginosis is more common amoung females who are sexually active, but it is not clear how sex changes the balance of bacteria. You can get Bacterial Vaginosis from toilet seats, bedding, swimming pools and touching objects around you.
Contraception
Contraception Choices

Several methods of contraception are available. The method you choose will depend on your general health, lifestyle and relationships. Contraceptives available include physical barriers and devices, hormonal (oral, implant and injectable) methods, sterilisation, emergency and ‘natural’ methods.
There are several methods of contraception available in Australia, including barrier methods (male and female condoms and diaphragms), hormonal methods (pills, vaginal rings, implants and injections), intrauterine devices (IUDs or coils), female and male sterilisation, emergency contraception and ‘natural’ methods.
Protect against Sexually Transmissable Infection
It is important to practice safe sex as well as to protect yourself against pregnancy. Not all methods of contraception provide protection against STIs. The best way to reduce your risk of STIs is to use barrier protection such as male and female condoms and dams (a thin piece of latex placed over the anal or vulval area during oral sex). Condoms can be used for oral, vaginal and anal sex to help prevent the spread of infections.
Physical barrier methods
Barrier methods of contraception stop sperm from getting into the womb (uterus). Options include male condom, Female condom and Diaphragm.
Male condom
This is a latex (or polyurethane) sheath that covers the erect penis and prevents semen entering the vagina. This is an effective form of contraception when used correctly.
Female condom
This is a loose polyurethane sheath with a flexible ring at each end that sits in the vagina and collects semen. It can be inserted several hours before intercourse and is stronger than the male latex condom, though insertion and use may take some practice.
Diaphragm
This is a soft, shallow rubber dome that fits in the vagina, covers the cervix and stops sperm from entering the uterus. The diaphragm must stay in place for at least six hours after intercourse and must be fitted and positioned correctly. Diaphragms must be fitted by a suitably trained doctor or nurse.
Intrauterine devices (IUD)
An IUD, sometimes known as a coil, is a small plastic device with added copper or hormones (Mirena) which is inserted into your uterus by a doctor. It can stay in the uterus for five to ten years (depending on the type used) and can easily be removed earlier if you want to become pregnant or are having problems.
Hormonal contraceptives – pills and vaginal rings
Hormonal contraception for women is available by prescription in the form of a pill (oral contraceptive) or a vaginal ring.
Combined pill
This is made up of synthetic forms of the hormones oestrogen and progesterone. The combined pill prevents ovulation, thickens cervical mucus to make it harder for sperm to enter the uterus and changes the lining of the uterus to make it less suitable for a fertilised egg to stick.
Vaginal ring
This contains similar hormones to the combined pill and works in the same way. A ‘one size fits all’ ring is inserted into the vagina and stays in place for three weeks. During that time, it slowly releases hormones that pass from the vagina into the bloodstream. It’s then removed and a new ring is inserted a week later.
Mini pill
This contains only a synthetic form of the hormone progesterone. It makes the cervical mucus thicker, which prevents sperm from entering the uterus. The mini pill must be taken every day at the same time and is not as effective as the combined pill. It’s usually suitable for women who either experience side effects from oestrogen or shouldn’t take it for health reasons.
Hormonal contraceptives – implants and injections
Hormonal contraceptives for women are also available as implants and injections. These methods are more effective than other hormonal methods, but may produce side effects and don’t protect against STIs.
Implanon
This is a hormone implant that is inserted under the skin at the inner side of the upper arm. It contains etonogestrel, a progesterone-like hormone that prevents ovulation and hinders sperm from entering the cervix by changing cervical mucus. The device is inserted by a doctor under local anaesthetic.
DPMA injections (Depo-Provera/Depo-Ralovera)
These are long-acting (12 to 14 weeks) injectable contraceptives containing the hormone progestogen. They prevent ovulation, block sperm by thickening the mucus made by the cervix and cause changes in the lining of the uterus to make it unsuitable for a fertilised egg to stick. DPMA injections are highly effective and provide a very private method of contraception.
Vasectomy
This involves blocking sperm by cutting the tubes they pass through from the testes to the penis.
Emergency contraception
Sometimes it is necessary to prevent pregnancy after sex, rather than before: for example, when a pill is forgotten or a condom breaks Emergency contraception, also known as the ‘morning after pill’, is a hormonal method of contraception that prevents or delays ovulation in that cycle. It may also stop a fertilised egg from sticking to the wall of the uterus.
There are different types of emergency contraception available. The most commonly used form, a single pill containing the hormone progestogen, can be prescribed by a doctor. Emergency contraception is best used within 72 hours of unprotected sex – the sooner within the 72 hours it is taken, the more effective it is. It can be taken up to 120 hours after unprotected sex, but will be less effective.
Natural methods
Natural family planning is based on an understanding of the menstrual cycle. Methods include monitoring cervical mucus changes, body temperature changes and rhythm or cycle calculations to help determine when a woman is most likely to be fertile each month.
The effectiveness of natural family planning varies in relation to whether one or a combination of methods is used. Confidence, correct use and effectiveness improve the longer the method is used. Natural family planning methods, however, do not protect against STIs.
Pregnancy Testing
Pregnancy Testing

The typical pregnancy test checks a woman's blood or urine for the presence of a substance called human chorionic gonadotropin (hCG). This is a hormone made by the placenta. When this hormone is present, it usually indicates that the woman is pregnant. Home pregnancy tests can give false positive or false negative results. If you suspect you could be pregnant, you can see your doctor for a pregnancy test. The doctor may perform a pregnancy test on your blood or urine. Your doctor can give you a blood pregnancy test as early as 11–14 days after ovulation. To perform a blood pregnancy test, the doctor draws blood from a vein in your arm. This blood is sent to a laboratory for testing. The results of most blood pregnancy tests take at least a couple of days. The laboratory then advises the doctor of the result.
Other reasons for a missed period
Pregnancy is not the only reason for a missed period. Other possible reasons include Breastfeeding, Emotional Stress, Severe Weight Loss, Server Dieting and Exercising and Obesity.
Menopause
Menopause
Menopause, also known as 'the change of life', is the final menstrual (monthly) period in a woman's life. Symptoms of menopause include no bleeding (period) for twelve months. Other symptoms may include hot flushes or night sweats, aches and pains, crawling or itching sensations on the skin, forgetfulness, irritability and reduced sex drive (libido). The decrease in female hormones may lead to a higher risk of osteoporosis and heart disease. Symptoms may be managed with lifestyle changes, hormone therapy and natural therapies. Most women reach menopause between the ages of 45 and 55, the average being around 50.
As you approach menopause, the production of hormones (for example oestrogen) by the ovaries starts to slow down. You may notice changes in your menstrual cycle for example cycles may become longer, shorter or totally irregular, Bleeding may become lighter or bleeding may become unpredictable and heavy (seek advice from your doctor).Eventually your hormone levels will fall to a point where menstruation (periods) will cease altogether and the menopause is reached.

Healthy Diet
Suggestions for managing menopause symptoms through diet include choosing a wide variety of foods, including plenty of fresh vegetables, fruits, cereals, whole grains and small portions of lean meat, fish or chicken several times a week, increase fluids and eat low fat dairy foods with high calcium content and decrease caffeine and limit alcohol (aim for 1–2 standard glasses or less per day).
Exercise
Regular exercise is important. At least 30–45 minutes on most days of the week will maintain your heart health and improve your general health, keep your bones healthy and prevent bone loss through osteoporosis, help maintain good balance and reduce the risk of injury from falls, provide a feeling of relaxation and wellbeing, possibly help improve hot flushes.
Understand your body’s changes
It is important to understand the changes your body is going through during menopause. There are many different sources of information available.
Avoid smoking
It’s important to avoid smoking because of the associated risk of osteoporosis, coronary heart disease and lung cancer (which may soon exceed breast cancer as the leading cause of death in women).
Think positive
Some women experience mood changes such as mild depression and irritability. These symptoms are often related to physical changes such as hot flushes, night sweats and poor sleeping. It’s important to keep a positive outlook. Consult with your doctor if you are experiencing any significant or persistent changes in mood.
Regular Pap tests and breast checks
You should have Two-yearly Pap tests and A two-yearly mammogram – this is a free, Australia-wide service for women over 40.
Hormone replacement therapy (also known as hormone therapy)
Hormone replacement therapy (HRT) effectively reduces many of the unpleasant effects of symptoms of the menopause and may be appropriate for short-term use in women with moderate to severe menopausal symptoms. Discuss the advantages and disadvantages of hormone therapy with your doctor.
Breast Screening
Breast Screening

Breast screening is the best method for detecting breast cancer early. This offers the best chance of successful treatment and recovery. A screening mammogram is a low dose x-ray of your breasts. Two-yearly mammography screening is most effective for women aged 50 to 69 years. Most women who have abnormal mammogram results don't have cancer.
Breast screening is the best method for detecting breast cancer in its earliest stages. Early detection offers the best chance of successful treatment and recovery. Screening mammograms use low dose x-rays of the breasts to detect cancers that are too small to be felt by you or your doctor.
Two-yearly mammography screening is most effective for women aged 50 to 69 years. Most women who have abnormal mammogram results don’t have cancer.
Free breast screening
BreastScreen Australia is a government-funded, national breast cancer screening program that provides high-quality mammography screening, particularly for women aged between 50 and 69 years. Women in this age group who attend BreastScreen are routinely re-invited for screening every two years. Screening mammography finds most cancers present at the time of the mammogram although, like other medical tests, it is not 100 per cent accurate.
If you have had breast cancer in the past, talk over screening options with your specialist, as the screening program may not be suitable for you.
Screening mammograms
A screening mammogram is a low dose x-ray of your breasts, used to detect unsuspected cancer at an early stage before symptoms appear. The mammogram is carried out by a radiographer. The mammogram provides a picture of the inside of your breast. The picture is then examined by a radiologist, who is trained to detect any abnormalities. Research has shown that regular mammography screening in women aged between 50 and 69 years can reduce deaths from breast cancer by up to one-third.
The BreastScreen program invites women aged between 50 and 69 years to have a free screening mammogram every two years. Women aged between 40 and 49 years or 70 and over may also be screened if they wish, but are not actively invited to the program and do not receive two-yearly reminder letters. Evidence indicates that breast screening is most effective in women aged 50 to 69 years.
Screening a whole population of women in a particular age group who do not have symptoms is different from the use of mammography to investigate symptoms in an individual woman. This is a diagnostic procedure. If you experience any symptoms or unusual changes in your breasts, see your doctor for diagnosis as soon as possible.
What to expect from a mammogram
While the mammogram is being taken, each breast will be compressed between two flat plates on the X-ray machine. Compressing the breast only lasts for a few seconds. Some women may experience discomfort, however, if you experience pain during the mammogram, you should let the radiographer know. You can also ask for the procedure to stop at any time. It is recommended that you advise your radiographer if you have sensitive breasts. She will work with you to make sure that the mammogram is as comfortable as possible.
Things to remember
- BreastScreen Australia offers free mammograms to women aged between 50 and 69 years.
- Women aged between 40 and 49 years or 70 and over may also be screened if they wish.
- Early detection and treatment can reduce illness and death from breast cancer.
- If you experience any breast symptoms or unusual changes, see your doctor without delay.
Incontinence
Incontinence
About bladder and bowel health
Healthy bladder and bowel habits can help you avoid bladder and bowel control problems such as incontinence. Incontinence can have a major impact on your quality of life. If you or someone you know is affected by incontinence it's important to remember that you're not alone - almost 4 million Australians are affected by incontinence, it affects both men and women, regardless of your age or background, it can be treated, managed and in many cases cured..
What is incontinence?
Incontinence is a term that describes any accidental or involuntary loss of urine from the bladder (urinary incontinence) or bowel motion, faeces or wind from the bowel (faecal or bowel incontinence).
Incontinence is a widespread condition that ranges in severity from 'just a small leak' to complete loss of bladder or bowel control. In fact, over 3.8 million Australians have bladder or bowel control problems for a variety of reasons. Incontinence can be treated and managed. In many cases it can also be cured.
Think you might have a problem?
If you experience bladder or bowel problems, but are not sure if you should seek help, try the questionnaire below.

Bladder and bowel questionnaire
- Do you sometimes feel you have not completely emptied your bladder?
- Do you have to rush to use the toilet?
- Are you frequently nervous because you think you might lose control of your bladder or bowel?
- Do you wake up twice or more during the night to go to the toilet?
- Do you sometimes leak before you get to the toilet?
- Do you sometimes leak when you lift something heavy?
- Do you sometimes leak when you exercise or play sport?
- Do you sometimes leak when you change from a seated or lying position to a standing position?
- Do you strain to empty to bowel?
- Do you sometimes soil your underwear?
- Do you plan your daily routine around where the nearest toilet is?
If You answered yes to any of these questions you may have a bladder or bowel control problem.
The first step is to talk to your doctor.
Urinary incontinence
Urinary incontinence (or poor bladder control) is a common condition, that is commonly associated with pregnancy, childbirth, menopause or a range of chronic conditions such as asthma, diabetes or arthritis.
Poor bladder control can range from the occasional leak when you laugh, cough or exercise to the complete inability to control your bladder, which may cause you to completely wet yourself. Other symptoms you may experience include the constant need to urgently or frequently visit the toilet, associated with 'accidents'.
There are different types of incontinence with a number of possible causes. The following are the most common stress incontinence, urge incontinence, overflow incontinence, functional incontinence.
Urinary incontinence can be caused by many things, but can be treated, better managed and in many cases cured. For this reason, it is important to talk to your doctor if you have any concerns.
Faecal incontinence
People with poor bowel control or faecal incontinence have difficulty controlling their bowels. This may mean you pass faeces or stools at the wrong time or in the wrong place. You may also find you pass wind when you don't mean to or experience staining of your underwear. About one in 20 people experience poor bowel control. It is more common as you get older, but a lot of young people also have poor bowel control. Many people with poor bowel control also have poor bladder control (wetting themselves).
Faecal incontinence can have a number of possible causes. The following are the most common weak back passage muscles due to having babies, getting older, some types of surgery or radiation therapy, constipation or severe diarrhoea.
Anxiety Disorders
Anxiety Disorders

Anxiety disorders are a group of psychiatric or psychological disorders. They include generalised anxiety disorders, social phobias, specific phobias – for example, agoraphobia and claustrophobia – panic disorders, obsessive compulsive disorder (OCD) and post traumatic stress disorder. Untreated anxiety disorders can lead to depression.
Anxiety disorders are common mental health problems that affect many people. Approximately 25 per cent of the population have an anxiety disorder that warrants treatment at some time in their life and up to another 25 per cent have less severe anxieties such as fears of spider and snakes.
Not all anxiety is a disorder
Everyone experiences anxiety and fear at times; they are normal and helpful human emotions that help us deal with danger. However, some people experience excessive and irrational anxiety, and worries that become ongoing and distressing and that interfere with their daily lives. This may indicate an anxiety disorder. Often there appears to be no obvious or logical reason for the way the person feels. This may make an anxiety disorder even more worrying to the sufferer.
Symptoms of anxiety disorders
The main features of an anxiety disorder are fears or thoughts that are chronic (constant) and distressing and that interfere with daily living. Other symptoms of an anxiety disorder may include:
- Panic or anxiety attacks or a fear of these attacks
- Physical anxiety reactions – for example trembling, sweating, faintness, rapid heartbeat, difficulties breathing or nausea
- Avoidance behaviour – a person may go to extreme lengths to avoid a situation that they think could bring on anxiety or panic.
Panic attacks are a common symptom
A panic attack is a sudden feeling of intense terror that may occur in certain situations or for no apparent reason. A panic attack does not mean a person is necessarily suffering an anxiety disorder. However, a panic attack is a common feature of each type of anxiety disorder. Symptoms of a panic attack may include:
- Shortness of breath
- Dizziness
- Rapid heartbeat
- Choking
- Nausea.
The cause of panic attacks is unknown but they may be related to a chemical response in the brain, caused by actual threatening or stressful events or by thinking about stressful events. The brain response leads to physiological changes in the body, such as shallow breathing and rapid heartbeat.
Panic attacks can be frightening. Some people say they feel like they are going to die or go crazy. People affected by panic attacks may avoid situations in which they think attacks might occur. In some cases, this may lead to the development of other anxiety disorders including agoraphobia.
Types of anxiety disorders
Anxiety becomes a disorder when it is irrational, excessive, too persistent and attached to situations that do not warrant it and when it interferes with the person’s daily life. Anxiety disorders include:
- Generalised anxiety disorder
- Social phobias – fear of social situations
- Specific phobias – for example a fear of open spaces (agoraphobia) or enclosed spaces (claustrophobia)
- Panic disorders – frequent and debilitating panic attacks
- Obsessive compulsive disorder
- Post traumatic stress disorder.
Generalised anxiety disorder
Generalised anxiety is excessive anxiety and worry about common issues. The focus of the anxiety might be family or friends, health, work, money or forgetting important appointments. A person may be diagnosed with a generalised anxiety disorder if:
- The anxiety and worry has been present most days over a six-month period
- The person finds it difficult to control their anxiety.
Social phobias
People with social phobia are afraid of being negatively judged or evaluated by others. This leads to fear of doing something that may humiliate them in public – for example public speaking, using public toilets, eating and drinking in public, writing in public, or any social encounters such as parties or workplaces.
Some social phobia sufferers may only fear one type of situation. Others may be concerned about several types of situations. This can lead them to avoid the feared situations, which can lead to severe isolation.
Specific phobias
A person with a specific phobia has a persistent and irrational fear of a particular object or situation. They may fear animals, places or people. Fear of the object or situation is so severe that a person may experience physical symptoms and panic attacks. Fears may include dogs, blood, storms, spiders or other objects or situations but, in all cases, the anxiety is both excessive and interfering.
The adult phobia sufferer usually knows that their fear is excessive or unreasonable. However, their need to avoid the object, place or person can significantly restrict their life.
Panic disorders
Panic or anxiety attacks are common. Panic disorders are less common; they affect about two per cent of the population. For a person to be diagnosed with a panic disorder, they would usually have had at least four panic attacks each month over an extended period of time. Often panic attacks may not be related to a situation but come on spontaneously.
Panic disorder may be diagnosed if panic attacks are frequent and if there is a strong and persistent fear of another attack occurring.
Obsessive compulsive disorder
People with obsessive compulsive disorder (OCD) have intrusive, unwanted and involuntary thoughts or impulses (obsessions). They also feel compelled to perform behavioural and mental rituals (compulsions) such as excessive handwashing, showering or checking. They are usually aware of the irrational and excessive nature of their behaviour.
Post traumatic stress disorder
Post traumatic stress disorder develops after someone is exposed to an extremely traumatic event. The event may be recent, such as a car accident or physical assault, or it may have occurred in the past, such as childhood sexual assault.
Reactions of grief, shock and anger are normal after traumatic events. However, people with post traumatic stress disorder experience severe, prolonged and intrusive reactions that dramatically affect their daily life. These may include intrusive thoughts or images of the traumatic situation that are as distressing, or more distressing, than the original event. Often people begin to avoid reminders of the trauma, including places or similar situations.
Anxiety disorders can have serious effects
An anxiety disorder may lead to social isolation and clinical depression, and can impair a person’s ability to work, study and do routine activities. It may also hurt relationships with friends, family and colleagues. Depression can be a serious illness with a high risk of self-harm and suicide.
Recovery is possible with treatment
Recovery from an anxiety disorder is possible with the right treatment and support. Effective treatments for anxiety disorders may include:
- Cognitive behavioural therapy – aims to change patterns of thinking, beliefs and behaviours that may trigger anxiety. Part of the therapy may involve gradually exposing a person to situations that trigger anxiety: this is called desensitisation.
- Anxiety management and relaxation techniques – for example hypnotherapy, meditation, breathing exercises and counselling.
- Medication – this may include antidepressants and tranquillisers.
Where can I get help?
- Your doctor
Depression

Depression
Depression is more than just a low mood - it's a serious illness. While we all feel sad, moody or low from time to time, some people experience these feelings intensely, for long periods of time and often without reason. People with depression find it hard to function every day and may be reluctant to participate in activities they once enjoyed.
Depression is one of the most common of all mental health problems. One in five people experience depression at some stage of their lives.
If you have any concerns please come and see one of our Gracemere Doctors or Registered Nurse for the best advice
Bipolar Disorder

Bipolar Disorder
Bipolar disorder, which used to be called manic depression, involves both periods of feeling low (depressed) and high (mania).
Most people experience a range of moods depending on what's happening in their lives. When good things happen, like getting a new job, going on a holiday or falling in love, it's natural to feel happy. On the other hand, when there are difficulties like losing a job or a loved one, having money or family problems, it can make a person feel down.
However, people with bipolar disorder experience extreme moods that can change regularly and may not relate to what is happening in their lives, although their mood swings may be triggered by certain events.
Postnatal Depression
Postnatal Depression

Adjusting to life as a mother can be difficult. In fact, for many women, having a baby is the most significant life-changing event they will ever experience. Adjusting to this major life change, as well as coping with the day-to-day stress of a new baby, can make some women more likely to experience depression at this time, particularly if they've experienced depression in the past.
Some women may experience depression during pregnancy and this is referred to as Antenatal Depression. Around 10 per cent of pregnant women in Australia experience antenatal depression and it is less common than depression which is experienced after the birth of a baby. Postnatal depression (PND) is the name given to depression that a woman experiences in the months after the birth of her baby. Postnatal depression affects almost 16 per cent of women giving birth in Australia. Perinatal depression is the collective term used to describe both antenatal and postnatal depression.
Postnatal Depression Awareness Week 2010 - November 14-20.
Arthritis
Arthritis

Arthritis occurs when joints or muscles become painful, stiff and swollen. Common types include osteoarthritis, rheumatoid arthritis, juvenile idiopathic arthritis, psoriatic arthritis, gout, ankylosing spondylitis and fibromyalgia. Exercise, medication and supportive therapies can help manage symptoms.
Sleep Apnea
Sleep Apnea

Sleep Apnea means absence of breath. Sleep apnea occurs when the airway from the mouth to the lung collapses during sleep. The person with sleep apnea may have hundreds of these episodes throughout the night, disrupting their sleep and reducing oxygen supply to vital organs. Sleep apnea is a common condition affecting about 5% of adults. Fortunately effective treatment is available and once treated the person with sleep apnea leads a normal healthy life.
People with sleep apnea usually snore loudly and have restless sleep. Sleep apnea is associated with heart attacks and stroke. Signs and symptoms such as snoring, obesity, observed apnea and sleepiness in the day may suggest that a person has sleep apnea but the best way to be really sure is with an overnight sleep study. In the sleep study the patient is wired up and attached to computers which measure their sleep, their breathing and oxygen levels. In many people sleep apnea results from being overweight. If this is the case, losing weight may help or even cure the apnea. In any case, losing weight may assist with cardiovascular disease such as high blood pressure and with diabetes management.
Eating Disorders
Eating Disorders

Low Self Esteem
Low Self Esteem
How do you see yourself?
Relationship Concerns
Relationship Concerns

We all have many different types of relationships - we are Partners, Parents, Siblings, distant relatives, friends, & colleagues.
Relationships usually involve some level of interdependence.
People in these various relationships tend to influence each other, in subtle or significant ways.
We share our thoughts and feelings, and engage in activities together.
Because of this interdependence, most things that change or impact one member of the relationship will have some level of impact on the other member.
Sometimes these relationships can be a cause of concern and we just need someone to talk to about it.
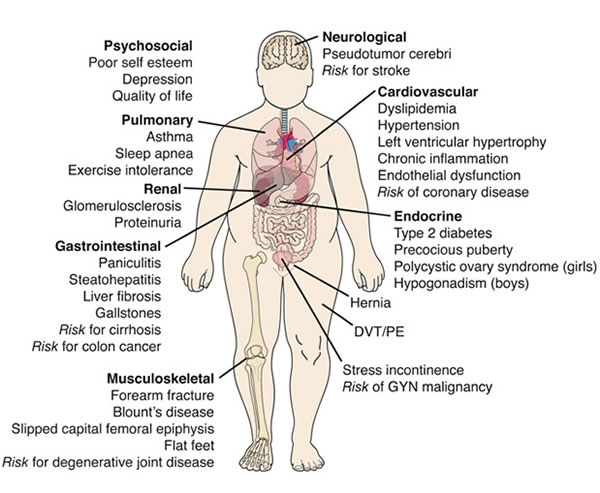
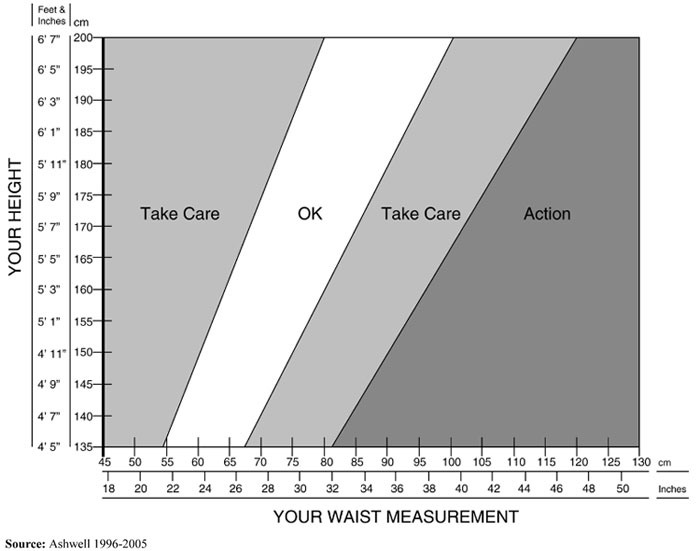
Obesity
Obesity
Some of the Health Risks associated with Obesity:
How do you measure up? See the chart below.
Stress
Stress
Life is busy, demanding and sometimes stressfull. Sometimes you may feel you need to find some balance again? Learning to recognise the signs and symptoms of stress can help us to reduce the harmful effects it can cause over a prolonged period of time.
|
|
Implanon
Implanon
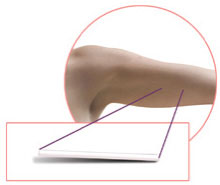
Birth control that lasts up to 3 years
Effective
- IMPLANON® is more than 99% effective: the chance of getting pregnant is less than 1 pregnancy per 100 women who use IMPLANON® for 1 year when IMPLANON® is inserted correctly.a
Discreet
- Most women can’t see IMPLANON® after insertion.
Long-acting
- One IMPLANON® provides up to 3 full years of contraceptive protection
Pre Natal & Antenatal Care
Pre Natal & Antenatal Care
The medical and nursing care of women and their children during pregnancy, childbirth and postnatal
The aim of good prenatal care is to detect any potential problems early, to prevent them if possible (through recommendations on adequate nutrition, exercise, vitamin intake etc), and to direct the woman to appropriate specialists, hospitals, etc. if necessary.
Pregnancy Planning